Unfortunately, pregnancy is often accompanied by numerous health risks and complications. Toxemia is one of such complications. This condition is often defined by high blood pressure yet its other signs are rather diverse and go from easily manageable to life-threatening.
What Is Toxemia?
Some women can develop toxemia after 4.5 months of pregnancy. In some rare cases, the disorder also develops after giving birth. This condition can cause unprecedented high blood pressure and protein in the urine. It can also lead to organ damage. Usually, a combination of symptoms can lead to such a diagnosis as toxemia or preeclampsia, as it is preferred in the medical community. It is also difficult to predict who may develop such a pregnancy complication.
The condition can develop rapidly and severely. Patients may suddenly begin to experience difficulty breathing and loss of consciousness and will require urgent hospitalization. On the other hand, some patients will proceed with their pregnancy (or after) with manageable toxemia signs. Here are the signs to look out for:
- high blood pressure;
- swollen ankles, hands, feet, and/or face;
- headaches;
- vision changes;
- nausea;
- breathing difficulty;
- fatigue;
- fainting.
Keep in mind that delivery may not end some or all of these symptoms, including their consequences.
Who Is at Risk of Developing Toxemia?
It is hard to make predictions about who will develop toxemia during pregnancy. Yet, there are certain factors and groups that are at high risk of developing this complication.
These are the most common of them:
- chronic high blood pressure or hypertension disorder;
- pregnancy at the age of 15-35;
- previous history of preeclampsia;
- diabetes;
- kidney disease;
- obesity and overweight;
- multiparity (carrying more than one fetus);
- damaged blood vessels;
- immune system diseases;
- first-time pregnancy.
Health care providers don’t have a precise answer on what causes toxemia. One of the opinions suggests that most abnormalities start in or due to the placenta. This organ is responsible for nourishing a fetus during pregnancy.
The Complications from Preeclampsia
People should never treat preeclampsia lightly. It requires constant monitoring and treatment. Otherwise, this condition can put the health and lives of a mother and baby in significant danger. In some extreme cases, toxemia can even be fatal. Also, it’s important to note that severe or life-threatening symptoms usually occur in early pregnancy. Hence, the risks of serious preeclampsia consequences slowly decrease as women proceed to their third trimester and after birth.
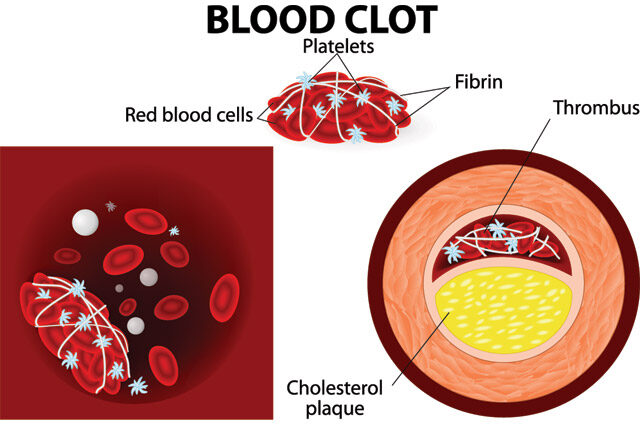
The typical consequences of this condition are highly unpleasant. Bleeding and organ damage (heart, lungs, kidneys, eyes, or liver) are common complications of toxemia. As a result, women experience higher risks of having a heart attack or stroke during or after pregnancy.
The condition can also cause the placenta to separate from the uterus walls. Such a detachment can affect the fetus’s development due to nutrients and oxygen deprivation. Eventually, this complication can result in premature birth, fetus death, and mother’s health complications.
In some extreme cases, a pregnant woman can suffer from eclampsia. This condition is characterized by seizures and coma, on top of the already mentioned above toxemia symptoms. Eclampsia is treatable, and people can fully recover from it. Yet, this condition can also carry brain damage and disability risks.
Lastly, patients with toxemia can develop HELLP syndrome. It’s a condition that causes the destruction of red blood cells, which can rapidly become life-threatening to the woman and fetus.
Diagnosing Preeclampsia
Checking for the signs of toxemia is a traditional part of prenatal care. Doctors will run tests and examinations every several weeks or so to make sure no early signs of toxemia development go unnoticed. Such tests include but are not limited to urine tests, frequent blood pressure readings, blood tests, fetal ultrasounds, and more.
Women in the group at risk but with no signs of the disorder will need to take aspirin in small doses to balance their blood pressure. Overall, regular check-ups should ensure an early diagnosis of the disease. The earlier it is discovered and treated, the less threatening it will be throughout the pregnancy.
Coping with Toxemia

There are various ways in which toxemia can be treated. It will depend on the severity of the symptoms and stage of the pregnancy. In case toxemia develops late into pregnancy and haslife-threatening symptoms, such as HELLP syndrome or eclampsia, obstetrics and gynecology personnel usually suggest early delivery. Most of the symptoms should resolve after birth. Though, medical care will still be necessary during the following weeks.
In addition, doctors highly recommend a healthy diet and exercise as a way to reduce any risks and manage pre-existing conditions of the disorder. More rest, strong and stable mental health, fewer stresses, and proper management of any chronic disorders can help control most risk factors of toxemia.
Toxemia During Pregnancy – Wrapping up
Any woman has a risk of developing toxemia symptoms after 20 weeks of pregnancy. They can appear at different times and of various severity, from light forms to life-threatening. Sometimes, some symptoms can carry on or suddenly appear even after delivery. There is still no clear understanding of which patient can develop toxemia beyond knowing the most at-risk group.
Fortunately, this condition can be treated, prevented, or managed throughout pregnancy. Numerous tests and checks can spot any early signs of toxemia, while bed rest, a nutritious diet, and reduced stresses can significantly decrease toxemia symptoms.